Choose Dr. Morton as your Joint Replacement Surgeon Today!
- Board-certified, Fellowship Trained Knee Surgeon
- Experienced Orthopedic Surgeon
- Nonoperative and operative treatments available
- High success rate in treating partial knee replacement
- Minimally invasive surgery
- Well-versed with modern techniques such as partial knee replacements and robotic-assisted joint replacements.
- Fellowship-trained and specialist in joint surgery and medicine
- Takes care of revision knee and hip replacements
Dental Work and Joint Replacements
When orthopedic surgeons discuss joint replacements with their patients, they often discuss the patient’s dental history. While dentistry and joint replacements may seem like very different fields, an infection in one can cause an infection in the other. For that reason, orthopedic surgeons will often prescribe antibiotics for their patients with joint replacements who are undergoing dental procedures. There are multiple professional societies that help clinicians decide when to use antibiotics before dental procedures in patients who have joint replacements.
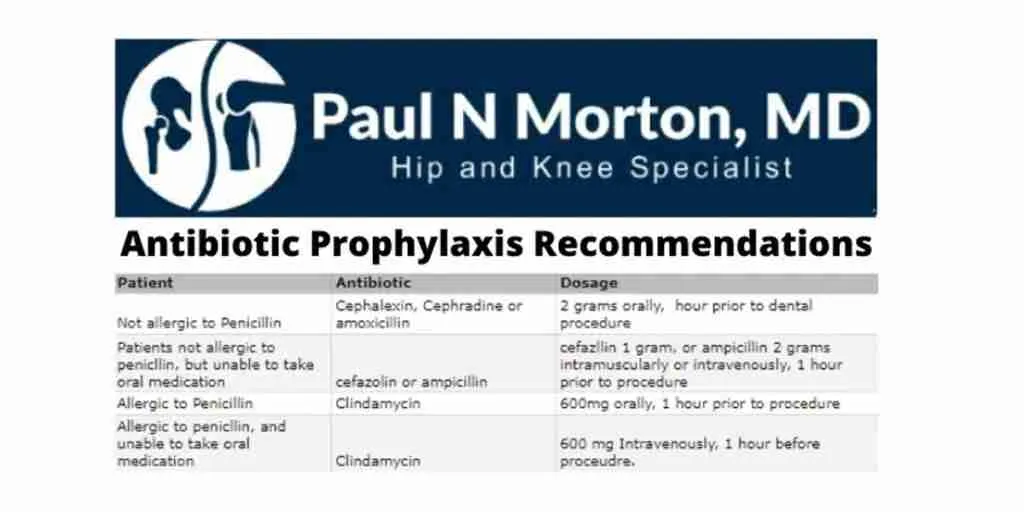
Antibiotics for dental work
Certain types of dental work can cause infections elsewhere in the body. There are many different types of bacteria in the mouth. Depending on the patient, the bacteria can cause an infection in different organ systems. For example, some patients can become bacteremic, meaning they develop a bacterial infection in their blood. Others may develop pneumonia, cardiovascular infections, or inflammatory conditions. Different patients have different risk factors.
Joint Replacement Infections
One of the risk factors for developing an infection after a dental procedure is having artificial hardware in one’s body. This includes joint replacements, the infection of which are called prosthetic joint infections (PJIs). There are many studies that examine the risks of PJIs with dental work. It is widely accepted by the medical community that there is a theoretical risk for bacteria to be released into the bloodstream through dental work and seed an infection in the prosthetic joint. In practice, however, many studies do not support the idea that dental procedures pose any greater risk to joints than everyday oral manipulation, such as brushing one’s teeth.
ADA and Orthopedic Society Antibiotic Recommendations
ADA
The American Dental Association (ADA) is the professional society for dentists. The ADA’s official recommendations are as follows: “For patients with prosthetic joint implants, prophylactic antibiotics are not recommended prior to dental procedures to prevent prosthetic joint infection.” They recommend abstaining from prophylactic antibiotics because they assert that there is no evidence that dental procedures are associated with PJIs. They also argue that there is no evidence to suggest that giving patients prophylactic antibiotics before dental procedures prevents PJIs. The ADA asserts that antibiotic resistance is a major concern, and the theoretical benefits are not enough to make up for this concern. However, they state that each patient should be considered individually, taking into account their personal risk factors.
American Academy of Orthopedic Surgeons (AAOS)
Just as the ADA is the professional society for American dentists, the AAOS is the professional society for orthopedic surgeons. They have released their own guidelines for surgeons when considering prophylactic antibiotics for dental procedures.
The AAOS states, “The practitioner might consider discontinuing the practice of routinely prescribing prophylactic antibiotics for patients with hip and knee prosthetic joint implants undergoing dental procedures.” They allow more discretion on the part of the physician. They assert that there is compelling evidence that oral procedures cause bacteremia, and that this bacterial blood infection could infect the joint hardware, particularly in the first 2 years after joint replacement. However, they agree with the ADA that the evidence for prophylaxis is not very strong and that the number of patients who need to take antibiotics to prevent one infection is very high.
Unlike the ADA, the AAOS delves more deeply into the patients that are an exception to their recommendations. For example, they state that immunocompromised patients are a special group. Immunocompromised patients do not have as strong of an immune system as their peers for a variety of reasons. The AAOS immunocompromised exceptions include patients with HIV/AIDS, cancer patients on immunosuppressive chemotherapy with signs of illness, other disease processes for which the patient is receiving immunosuppressive medications, and bone marrow recipients in a certain time frame. They also encourage physicians to include diabetes when considering the risk for infection. People with diabetes are more likely to have infections with their elevated blood sugar and compromised vasculature.
Uncertainty
As their statement indicates, the AAOS feels that there may be a role for antibiotics for prophylactic purposes. They give the individual surgeon more leeway when deciding. Specifically, their 310-page guidelines report describes the different studies that address antibiotics before dental procedures in patients with joint replacements. They argue that many of the studies that suggest that physicians do not need antibiotic prophylaxis have limited evidence to support that suggestion. They argue that because the consequences of getting an infection can be devastating and the scientific literature against antibiotic prophylaxis is weak, surgeons can use their own discretion.
As stated above, the consequences of infection can be significant. If a joint gets infected, the patient may have to undergo another surgery to remove the joint and infected tissue. The patient may have to go through multiple surgeries to remove the infection. The infection could spread to other places in the body. In all cases, the patient would have to receive antibiotics for a longer period of time than if they had just taken the prophylactic antibiotics. Surgeons are wary of infections because of these drawn-out consequences. They may wish to save their patients from these possibilities.
Conclusion
It is important to treat each patient as an individual and to share in that decision-making with the patient. Both of the societies provide evidence that supports recommendations, for and against dental prophylaxis. If you have questions regarding dental prophylaxis following your hip or knee replacement, talk with Dr. Morton about your antibiotic use.
Works Cited
Antibiotic Stewardship,www.ada.org/en/member-center/oral-health-topics/antibiotic-stewardship.
Lockhart, Peter B., et al. “Evidence-Based Clinical Practice Guideline on Antibiotic Use for the Urgent Management of Pulpal- and Periapical-Related Dental Pain and Intraoral Swelling.” The Journal of the American Dental Association, vol. 150, no. 11, 2019, doi:10.1016/j.adaj.2019.08.020.
OrthoGuidelines, www.orthoguidelines.org/go/auc/default.cfm?auc_id=224995&actionxm=Terms.
“Orthopaedic Implant Infection in Patients Undergoing Dental Procedures.” AAOS, aaos.org/quality/quality-programs/tumor-infection-and-military-medicine-programs/orthopaedic-implant-infection-in-patients-undergoing-dental-procedures/.
Sollecito, Thomas P., et al. “The Use of Prophylactic Antibiotics Prior to Dental Procedures in Patients with Prosthetic Joints.” The Journal of the American Dental Association, vol. 146, no. 1, 2015, doi:10.1016/j.adaj.2014.11.012.
“The Practitioner Might Consider Discontinuing the Practice of Routinely Prescribing Prophylactic Antibiotics for Patients with Hip and Knee Prosthetic Joint Implants Undergoing Dental Procedures.” OrthoGuidelines, www.orthoguidelines.org/guideline-detail?id=1021.