Avascular Necrosis of the Hip

Content
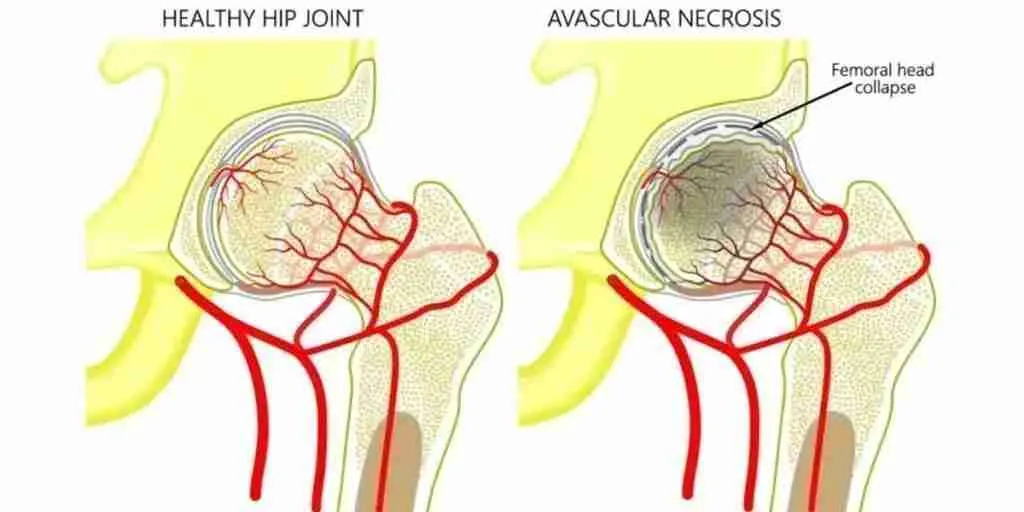
How does Avascular Necrosis (AVN) of the Hip Occur?
What Causes AVN?
As stated above, avascular necrosis has many causes. In fact, most researchers believe that the condition is caused by a constellation of factors acting at once to create the perfect storm. This condition can occur in children or adults and can be caused by medications, conditions, or other factors.
Two common causes that cause avascular necrosis are glucocorticoids and alcohol. Glucocorticoids, commonly known as steroids, are used to treat many medical conditions. In some people, they can impair blood flow to the femoral head and cause necrosis of the bone. Excessive alcohol use also causes avascular necrosis. Scientists believe this is due to changes in stress levels, an increase in fat, and sluggish blood flow.
Many medical conditions are associated with avascular necrosis of the hip. These include Lupus, the presence of antiphospholipid antibodies, Sickle Cell Disease, Gaucher Disease, Decompression Disease, Acute Lymphoblastic Leukemia, and kidney transplants. Avascular necrosis in children can be due to a congenital condition called Legg-Calvé-Perthes disease. Additionally, trauma, such as falling or being hit by a car, puts both adults and children at risk for avascular necrosis.
How is AVN Diagnosed?
When physicians suspect avascular necrosis, they turn to imaging. An X-ray is the best initial test and will show changes in the bone that are characteristic of avascular necrosis. The physician then orders Magnetic Resonance Imaging (MRI). An MRI can accurately visualize the necrotic bone and confirm the diagnosis.
What are my Treatment Options for Avascular Necrosis of the Hip?
Avascular necrosis can be difficult to treat depending on the patient. The first step is to identify the cause of the necrosis and stop or manage the offending agent. This also includes optimizing other risk factors that impede blood flow, including smoking. Early in the disease, some physicians recommend starting with non-operative management. Non-operative management includes reducing weight-bearing by using crutches and using medications to reduce pain and maintain bone density. However, non-operative management has been found to be ineffective at halting the progression of the disease. Therefore, many people turn to operative management.
Operative management can be divided into two classes: joint-preserving procedures and joint replacement procedures. One option for a joint-preserving procedure is called core decompression. This is when the surgeon uses a tool to decompress the femoral head to restore blood flow. They often then use a bone graft to fill in the parts of the bone that have died.
Researchers have examined the success rate of core decompression with and without bone grafting have mixed results. Many studies have demonstrated that patients have significant pain relief with core decompression. Only certain patients reported excellent outcomes from core decompression, particularly those that had the procedure done early in the disease before the bone collapsed. Other patients had less success.
When joint-preserving procedures are not successful, the next option is a joint replacement. Total hip replacements are generally successful with a low revision rate. Because the revision rate is low, some surgeons prefer total hip replacements over joint-preserving procedures. Other surgeons prefer to be more selective with who receives a total hip replacement depending on their disease progress and lifestyle.
Conclusion
Avascular necrosis of the hip is a condition that causes pain and reduced mobility of the hip. Treatment is complicated and depends on the patient, his or her lifestyle, and his or her risk factors. If you suffer from avascular necrosis of the hip, schedule an appointment to talk with Dr. Morton to determine the best course of action for you.
Frequently Asked Questions About Avascular Necrosis (FAQ)
Long-distance travel should usually be avoided until at least after your initial post-operative visit with your surgeon. The concern with long-distance travel is the possibility of the development of a blood clot, or missing a postoperative complication.
Once you are on a long trip, Dr. Morton recommends that you get up to stretch or walk at least once per hour during a long trip. Taking 81mg of aspirin daily is a useful adjunct. Dr. Morton recommends starting aspirin 2 days before your trip, and 2 days after your trip to avoid blood clots. You may want to talk with your primary care physician if you have a history of stomach ulcers, allergies, blood clots, or bleeding disorders. Usually, patients will desire an aisle seat or a lay-flat seat for long distances during their initial recovery.
The answer varies from patient to patient, and whether you have surgery on the right leg or the left leg. As a general rule, you cannot drive if you are on narcotics or unsafe on the road. Patients on average are able to return to driving between 2 and 6 weeks after surgery. I usually advise my patients that if they feel like they wouldn’t be able to stop in the event of an emergency or if a pedestrian suddenly decided to cross the road in front of the car, they should not drive. Practice on a parking lot before driving on the road.
This is a complex question depending on what job type you are doing.
Desk job: I tell most patients that they will feel well enough to begin working around two weeks after surgery. Some patients who are gung-ho will even start working immediately after surgery.
Light Labor: Light labor that requires frequent walking or light lifting. Some patients may require 6 weeks to 3 months before returning to work. Close monitoring will be needed to help you determine when you are safe.
Heavy labor: Construction and other types of manual labor usually requires at least 3 months of recovery. Some patients will have to change their careers depending on their demands. Talk with your surgeon before returning to work.
Tobacco use is known to be a significant risk factor for loosening, infection, or wound healing problems. Minimizing your tobacco use or quitting before surgery will make a significant impact. If you are able to quit for life, you will significantly reduce your risk of other complications to your overall health as well. Learn more about tobacco effects on joint replacements here.
The arthritic pain from before surgery is usually removed following hip replacements. Many patients tell me they have minimal to no pain following surgery initially. Some patients have soreness for up to 2 months. Again, I have noticed that many patients have a lower amount of pain through the anterior approach.
Hip replacement recovery is variable. Many patients are feeling good at 6 weeks. It may take 3 months to a year before you completely recover from your hip replacement. The anterior hip replacement consistently allows for a quicker recovery.
50% of people who are diagnosed with AVN of the hip undergo surgery within 3 years of their diagnosis. If there is bone collapse, this process occurs sooner.
Related Pages
Faster Recovery: The Subvastus Advantage in Knee Replacements
Total knee replacement (TKR) surgery is a transformative procedure for patients suffering from severe knee arthritis or injury. Among the various surgical techniques, the subvastus approach, Quadriceps Sparing Approach, stands out as a minimally [...]
Knee Replacement Success Rate
Introduction Knee replacement surgery, or knee arthroplasty, is a procedure that has transformed the lives of millions of patients suffering from severe knee pain and mobility issues. Traditionally, the success of such surgeries has [...]
Choosing the Right Specialist for Regenerative Medicine: Ensuring Safety and Efficacy
Regenerative medicine is a rapidly advancing field in healthcare, promising innovative treatments that help regenerate tissues, alleviate pain, and restore function. These treatments require technical knowhow when obtaining platelet rich plasma, bone [...]
Demystifying PRP Therapy: Understanding the Science Behind Platelet-Rich Plasma
In the quest for advanced healing techniques, Platelet-Rich Plasma (PRP) therapy emerges as a beacon of hope for those suffering from various orthopedic conditions, including osteoarthritis and tendon injuries like tennis elbow. This cutting-edge [...]
Moving Forward without Cement: The Pros and Cons of Uncemented Knee Replacements
Introduction Modern medicine continues to break new ground, redefining what's possible. One field where innovation is unceasing is orthopedic surgery, and one of the groundbreaking procedures reshaping the sector is uncemented knee replacements. As [...]
Speedy Recovery: Practical Tips for a Faster Recovery After Knee and Hip Replacement
Introduction Hip and Knee Arthroplasty, more commonly known as hip and knee replacement surgery, is a widely performed procedure that offers a new lease on life for individuals grappling with severe knee conditions, including [...]