Hip replacements provide the ability to reduce severe pain and stiffness while improving function in over 400,000 people in the United States each year. There are different approaches your surgeon may take when replacing the hip joint. Read further to learn some tips and tricks to follow to ensure you have a speedy and healthy recovery.
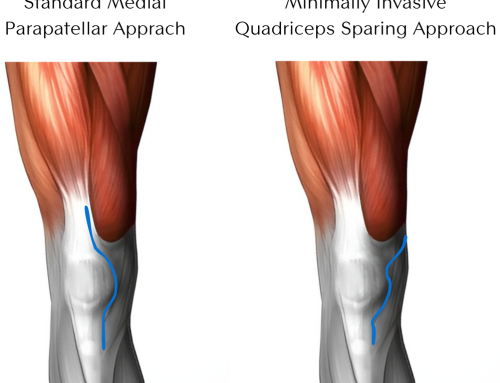
There are a few differences in the beginning stages of recovery depending on the approach. Depending on your body shape, size, and status of your hip, your surgeon may approach the hip from posterior (the back side) or anterior (the front side).
The posterior approach requires six weeks of restrictions on how much you can flex your hip, rotate it in, and cross it over midline. In the anterior approach, your limitations are less severe. Patients usually need to be mindful of passive stretching of the front of their hip joint, but it is much less common to require restrictions. The specific details should be discussed with your surgeon and Physical Therapist. Your Physical Therapist will also work with you throughout your recovery, providing guidance and encouragement, and helping you reach your goals.
Now, let’s look at the first year of recovery after a hip joint replacement.
The First Week
After you awake from surgery, you may begin walking with a walker as tolerated. Walking and other gentle movements are encouraged to help reduce swelling, manage pain, and start the recovery process. However, right now is the time to avoid adding extra weight or resistance to your exercises. You can begin low-intensity isometric exercises right away, and your Physical Therapist will teach you the best way to do these.
Before your surgery, you should talk with your surgeon about any movement restrictions you may have. It is important to remember these restrictions, not just in the first few days but throughout the first six weeks. You will have to be careful with transferring, moving around in bed, sleeping, dressing, and other normal daily activities. With the anterior approach, the restrictions fall outside of the regular motions expected in every-day life.
Within the first week, you will also want to monitor the bandage over the incision to ensure there is not excessive drainage, swelling, or redness. Keep your surgeon informed about what seems out of the ordinary.
Continuous cryotherapy (ice) throughout the first week, along with following the prescribed medication schedule, will significantly help with pain, allowing you to work on rehabilitation without increasing pain levels. This is the first crucial step in a speedy recovery.
It is essential to manage your pain and swelling with cryotherapy, pain medication, and gentle movements. Suppose you get out of control with your pain levels early on. In that case, you risk slowing down your recovery, losing out on gaining your full range of motion, a regular walking pattern, and your full functional ability.
The First Month
You will have a follow-up visit with your surgeon to ensure everything is healing and remove the dressing and bandage.
You may continue to walk with an assistive device throughout the first month, such as a walker or cane. Still, you can discontinue use of this once you feel comfortable, stable, strong. You can move without limping or other compensatory patterns. However, one tip for a speedy recovery in this timeframe is not discontinuing the assistive device too soon. If you feel unstable, continue to use your walker as you do not want to fall. A fall could slow your recovery down, and worse, even cause your hip replacement complications if you were to fall onto that side.
Strengthening is significant during this phase. Exercises to promote the surgical leg’s strength will have to be prescribed as tolerated and progressed based on pain and mobility. However, the rest of the body, including the core and other leg, can be addressed with strengthening exercises to promote better posture, stability, and balance.
Balance is also a critical piece of recovery. Balance training will improve your balance, which results in a decrease in your fall risk. It also improves your proprioception, your ability to know where your new hip is, how it is positioned, and how it works with the rest of your body.
Range of motion and flexibility are also essential. But this may be slower to address than strengthening or balance as you may have restrictions on how your leg can be moved, based on the approach taken to replace your hip.
Your Physical Therapist will be the one to initiate mobility exercises as they can passively move your hip around, stopping before they go too far. Then over time, as this passive movement improves without pain and as you are outside of your six-week restrictions, you may start to move and stretch your hip further, using pain as your guide.
The ability to walk with a regular gait pattern will also help to speed up your recovery. After having a hip replacement, it is easy to get into the habit of swinging your leg out to the side instead of swinging your leg forwards when you walk. Put in the time and practice early on in recovery to develop the strength and the correct habits and movement patterns. That way, you will speed up your recovery as you won’t have to “fix” this later on down the road.
The First 3 Months
You will start to feel more like yourself during this timeframe as more fun and functional activities can resume. You should still monitor your pain and swelling throughout this timeframe, using these two symptoms to help guide treatment.
Now that you can move your hip into an unrestricted range of motion, the number of exercises and activities you can perform can expand. Exercises added during this time frame include stairs, squats, lunges, bike riding, swimming, walking, etc. Since you have not done activities like these for a while, it is best to work with your Physical Therapist on a gradual progression in returning to these movements and actions.
That is a vital tip for a speedy recovery during this time frame, don’t do too much too soon. Excessive joint loading before you have adequately progressed can cause increased pain, swelling, and stiffness.
Continue to work on your core and your other leg, developing your whole body’s strength and endurance. Balance exercises can also become more challenging, mimicking work or activities you want to return. Hiking, walking on the sand, and yard work are examples of activities where you may need to walk around on uneven surfaces without falling.
The Final 9 Months of Recovery
Typically after the first three months of recovery, you may be able to discharge from Physical Therapy and begin your own independent home exercise program. With a focus on watching for pain, swelling, stiffness, and any limp or compensatory movement while walking, you should be able to progress on your own at home safely.
If you start to notice any of those symptoms previously listed, reach out to your surgeon or Physical Therapist for guidance on what to do. That is an essential tip for a speedy recovery. Don’t forget that you can reach out to your healthcare team if you encounter any setbacks. They are here to help guide you and help you return to whatever it is that you want to do.
During this time, you will be able to return to more challenging activities that you used to previously enjoy such as golf, doubles tennis, biking, low impact aerobics, swimming, snorkeling, scuba diving, yoga, or paddling.
Now is the time when you realize how much of your life you were missing before.
If you are experiencing hip pain and are wondering if a hip replacement is right for you, reach out to Dr. Morton for a full evaluation.