Interested in Deformity Correction? Book an Appointment.
Choose Dr. Morton as your Deformity Correction Surgeon Today!
- Experienced Surgeon: Dr. Paul Morton brings years of expertise in adult reconstruction surgery , ensuring high success rates and improved patient outcomes.
- Fellowship-Trained Specialist: Dr. Morton is fellowship-trained in adlt reconstruction.
- Cutting-Edge Technology: We utilize the latest advancements in orthopedic surgery including robotics, custom guides and implants to provide precise and effective treatments.
- Patient-Centered Care: Our team is dedicated to offering compassionate care, addressing your concerns, and supporting you throughout your treatment journey.
- Comprehensive Services: From diagnosis to postoperative care, we offer a full spectrum of services to ensure a seamless and successful treatment experience.
Introduction
Limb deformities can significantly impact a person’s quality of life, affecting mobility, appearance, and overall function. These deformities can arise from various causes, including congenital issues, disease processes, and trauma. In this post, we will explore two common types of deformities, varus and valgus, along with post-traumatic deformities, their causes, implications, and potential treatments.
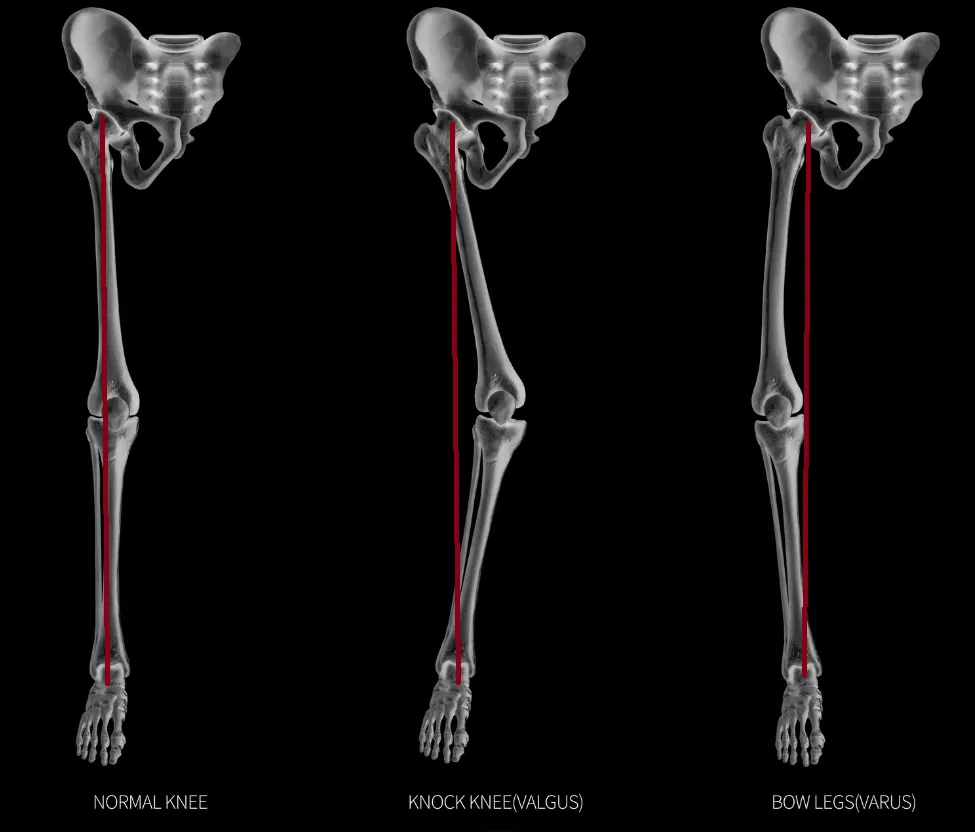
Varus and Valgus Deformities
Varus and valgus deformities refer to angular deviations of a limb, commonly seen in the knees but also present in other joints such as the hips and ankles.
Varus Deformity
Definition: A varus deformity occurs when a limb is angled inward, causing the distal part of the limb to point towards the midline of the body. This is commonly known as “bow-leggedness” in the context of the knees.
Causes:
- Congenital Conditions: Conditions like Blount’s disease can cause varus deformities.
- Rickets: A disease resulting from vitamin D deficiency can lead to improper bone formation.
- Osteoarthritis: Degenerative changes in the knee joint can lead to varus alignment as the medial compartment of the knee wears down more than the lateral compartment.
Implications:
- Joint Stress: Increased stress on the medial aspect of the knee joint can accelerate wear and tear, leading to osteoarthritis.
- Gait Abnormalities: Changes in the walking pattern can result in further musculoskeletal issues.
Treatment:
- Conservative Management: Physical therapy, orthotics, and bracing can help manage symptoms and improve function.
- Surgical Intervention: High tibial osteotomy (HTO) is a common procedure to realign the knee joint by cutting the tibia (shinbone) and reshaping it. In severe cases, knee replacement surgery may be necessary.
Valgus Deformity
Definition: A valgus deformity occurs when a limb is angled outward, causing the distal part of the limb to point away from the body’s midline. This is often called “knock-knees” when it affects the knees.
Causes:
- Genetic Factors: Some individuals are predisposed to valgus alignment due to their genetic makeup.
- Rheumatoid Arthritis: This inflammatory condition can lead to joint damage and valgus deformities.
- Injury: Previous injuries to the knee can result in a valgus alignment over time.
Implications:
- Joint Stress: The lateral compartment of the knee experiences increased pressure, potentially leading to degenerative changes.
- Functional Limitations: Difficulty with certain activities and an increased risk of falls.
Treatment:
- Non-Surgical Approaches: Physical therapy and bracing can help manage symptoms.
- Surgical Options: Distal femoral osteotomy (DFO) is a procedure in which a cut is made in the femur (thighbone) to realign the knee. Knee replacement surgery may also be indicated for severe cases.
High Tibial Osteotomy (HTO)
High Tibial Osteotomy (HTO)
Definition: High tibial osteotomy (HTO) is a surgical procedure that involves cutting and reshaping the upper part of the tibia (shinbone) to realign the knee joint. It is commonly used to correct varus deformity (bow-leggedness) to relieve pain and improve function in patients with medial compartment osteoarthritis.
Indications:
- Medial compartment osteoarthritis with varus alignment
- Younger, active patients who are not yet candidates for knee replacement
- Patients with localized cartilage damage
Procedure:
- Preoperative Planning: Detailed imaging studies, including X-rays and MRIs, assess the alignment and condition of the knee joint. The surgeon then plans the precise location and angle of the osteotomy.
- Anesthesia: The procedure is performed under general or spinal anesthesia.
- Incision and Exposure: A surgical incision is made on the front or side of the knee to expose the upper part of the tibia.
- Osteotomy: The surgeon makes a controlled cut in the tibia, creating a wedge-shaped opening. Depending on the type of osteotomy, the wedge may be opened (opening wedge osteotomy) or closed (closing wedge osteotomy).
- Realignment: The tibia is realigned to shift the weight-bearing axis from the damaged medial compartment to the healthier lateral compartment.
- Fixation: The bone is stabilized using plates, screws, or a combination of both to hold the tibia in its new position.
- Closure: The incision is closed with sutures or staples, and a sterile dressing is applied.
- Hospital Stay: Patients may be discharged as an outpatient, same-day surgery. More complex patients may require hospitalization.
- Weight Bearing: Initial non-weight-bearing with crutches or a walker, gradually progressing to full weight-bearing as healing occurs.
- Physical Therapy: Essential for restoring range of motion, strength, and function. Therapy usually starts soon after surgery and continues for several months.
- Full Recovery: Returning to full activity can take 6-12 months.
Distal Femoral Osteotomy (DFO)
Definition: Distal femoral osteotomy (DFO) is a surgical procedure that involves cutting and reshaping the lower part of the femur (thighbone) to realign the knee joint. It is commonly used to correct valgus deformity (knock-knees) to alleviate pain and improve function in patients with lateral compartment osteoarthritis.
Indications:
- Lateral compartment osteoarthritis with valgus alignment
- Younger, active patients who are not yet candidates for knee replacement
- Patients with localized cartilage damage
Procedure:
- Preoperative Planning: Detailed imaging studies, including X-rays and MRIs, assess the alignment and condition of the knee joint. The surgeon then plans the precise location and angle of the osteotomy.
- Anesthesia: The procedure is performed under general or spinal anesthesia.
- Incision and Exposure: A surgical incision is made on the knee’s outer side to expose the femur’s lower part.
- Osteotomy: The surgeon makes a controlled cut in the femur, creating a wedge-shaped opening. Depending on the type of osteotomy, the wedge may be opened (opening wedge osteotomy) or closed (closing wedge osteotomy).
- Realignment: The femur is realigned to shift the weight-bearing axis away from the damaged lateral compartment to the healthier medial compartment.
- Fixation: The bone is stabilized using plates, screws, or a combination of both to hold the femur in its new position.
- Closure: The incision is closed with sutures or staples, and a sterile dressing is applied.
- Hospital Stay: Patients may be discharged on the same day, but sometimes they may stay there for a few days.
- Weight Bearing: Initial non-weight-bearing with crutches or a walker, gradually progressing to full weight-bearing as healing occurs.
- Physical Therapy: Essential for restoring range of motion, strength, and function. Therapy usually starts soon after surgery and continues for several months.
- Full Recovery: Returning to full activity can take 6-12 months.
Post-Traumatic Deformities
Post-traumatic deformities result from injuries that heal improperly, leading to abnormal alignment and function of the affected limb.
Causes
- Fractures: Incomplete or improper healing of fractures can lead to angular deformities, limb shortening, or rotational abnormalities.
- Soft Tissue Injuries: Severe injuries to ligaments, tendons, and muscles can alter the biomechanics of the limb, resulting in deformities over time.
- Infections: Infections after trauma can disrupt normal bone healing and lead to deformities.
Implications
- Pain and Disability: Deformities can cause chronic pain, limited mobility, and functional impairment.
- Osteoarthritis: Abnormal joint loading can accelerate the development of osteoarthritis.
- Psychosocial Impact: Visible deformities can affect a person’s self-esteem and mental health.
Treatment
- Early Intervention: Prompt and appropriate management of fractures and soft tissue injuries is crucial to prevent deformities.
- Corrective Surgery: Osteotomies, limb lengthening, and joint replacement can address established deformities.
- Limb Lengthening: This process involves gradual bone lengthening using devices such as the Ilizarov fixator, helping to correct limb length discrepancies.
- Rehabilitation: Comprehensive rehabilitation programs are essential to restore function and improve outcomes post-surgery.

Congenital Deformities
Congenital deformities are present at birth and can result from genetic factors or developmental issues during pregnancy.
Causes
- Genetic Disorders: Conditions like achondroplasia and osteogenesis imperfecta can lead to limb deformities.
- Developmental Issues: Problems during fetal development, such as amniotic band syndrome, can cause limb deformities.
- Environmental Factors: Maternal health issues or exposure to harmful substances during pregnancy can contribute to congenital deformities.
Implications
- Functional Limitations: Depending on the severity, congenital deformities can lead to significant mobility and functional challenges.
- Psychosocial Impact: Visible deformities can affect a child’s self-esteem and social interactions.
- Long-term Health Issues: Some congenital deformities may require ongoing medical treatment and monitoring.
Treatment
- Early Diagnosis: Prenatal screenings and early postnatal assessments are crucial for identifying congenital deformities.
- Multidisciplinary Approach: Treatment often involves a team of specialists, including orthopedic surgeons and physical therapists.
- Surgical Intervention: Procedures such as osteotomies, corrective surgeries, and limb lengthening can improve function and appearance.
- Therapy and Support: Physical and occupational therapy, along with psychological support, play a vital role in managing congenital deformities.
Learn More
Conclusion
Limb deformities, whether varus, valgus, post-traumatic, or congenital, pose significant challenges to those affected. Understanding the causes and implications of these deformities is crucial for effective management. Advances in medical and surgical treatments offer hope for improved function and quality of life for individuals with these conditions. If you or someone you know is experiencing symptoms of a limb deformity, consult with a healthcare professional to explore the best treatment options.
Schedule a Consultation
Related Pages
Personalized Alignment In Knee Replacement Surgery
Knee replacement surgery has long been a solution for patients who have severe arthritis or joint degeneration. Traditionally, the procedure has involved using standardized techniques to position the knee implant. However, personalized alignment in knee [...]
Hiking After Knee Replacement: Tips for Staying Active
Knee replacement surgery can be life-changing, offering significant relief from pain and improved mobility. However, returning to physical activities like hiking may seem daunting for many. However, hiking after knee replacement is possible—and even beneficial [...]
Uncemented Knee Replacement: What Patients Should Know
Knee replacement surgery has evolved significantly over the years, with various techniques and approaches tailored to meet individual patient needs. Among these, uncemented knee replacement is gaining attention as an alternative to the traditional [...]
How Much Does A Hip Or Knee Replacement Cost?
Understanding Your Expected Bills Hip or knee replacement surgery is a transformative procedure that can significantly improve the quality of life for individuals with severe arthritis or joint damage. However, the financial aspect [...]
Cost of Total Knee Replacement in Hawaii for Medicare Patients: How to Save Money with Outpatient Surgery Centers
Total knee replacement (TKA) is a life-changing procedure for patients suffering from severe arthritis or knee dysfunction. With advancements in surgical techniques, many TKAs are now performed on an outpatient basis, allowing patients to [...]
Understanding Post-Traumatic Arthritis After ACL Reconstruction
Anterior Cruciate Ligament (ACL) injuries are a common occurrence, especially among athletes and physically active individuals. While ACL reconstruction is a widely accepted procedure to restore knee stability and function, it is important to [...]