In hip and knee replacement surgery, the hip and knee prostheses are made from metal. Metal can be a problem for those with hypersensitivity to metals, especially those with nickel allergies. Other materials may be used in place of nickel to make the joint, but they come with their own set of drawbacks. If you are concerned about a metal allergy, get an appointment with Dr. Morton and get tested today.
What metals are typically in a knee replacement?
There are several metal alloys typically found in knee replacements, including cobalt, chromium, titanium, and nickel. These metals combine long-term durability with biocompatibility.

What is a metal allergy?
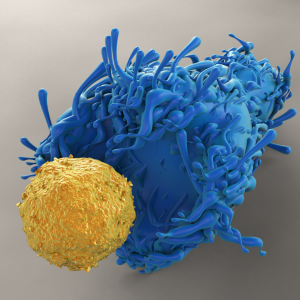
Metals found in knee prostheses can activate your immune system, leading to implant failure. Metal hypersensitivity (also known as metal allergy) is considered a Type IV hypersensitivity. This is a type of allergy where the presentation of symptoms is delayed (not an immediate reaction, as in anaphylaxis or allergic shock).
There are two phases to a type IV hypersensitivity. During the first phase, your body becomes sensitized to the metal. Eventually, the proteins in your body bind to the metal, forming antigen-hapten complexes. The antigen-hapten complexes are then presented to T-cells, macrophages, and other immune cells in your synovial tissue.
These T-cells are responsible for various symptoms, including increased swelling, stiffness, pain, loss of motion, and a rash.
Metal hypersensitivity is controversial, as many orthopedic surgeons do not believe in metal allergies. Many orthopedic surgeons will consider using unique implants for patients who notice an allergic contact dermatitis reaction after their skin touches cheap metals.
How common is a metal allergy in the population?
In the general population, it is estimated that the prevalence of a nickel allergy is 13%, cobalt is 2% and chromium is 1%. Allergy to other metals is fairly rare. However, the presence of a skin allergy alone, may not dictate an allergic reaction to a knee replacement. If you notice a skin rash after wearing costume jewelry, you may be allergic to nickel. Please inform Dr. Morton if you have contact dermatitis secondary to a nickel allergy.
How do I know if I have a metal allergy?
Patients considering knee replacement are often asked about their history of allergies. If patients note that they have a contact allergy following direct contact with metal exposure, such as with costume jewelry, they may have a nickel allergy. Tattoo inks also have metal salts in them, so someone who develops contact dermatitis after getting a tattoo might be at risk of a cobalt or nickel allergy.
Contact Dermatitis
Symptoms of a metal allergy can take from 4 weeks to 2 years to develop symptoms after surgery.
Before diagnosing an allergic reaction to metal, other causes of persistent pain should be ruled out, such as:
- Infection
- Midflexion instability
- Malalignment
- Patella tracking issues
- Implant loosening
- Metallosis
To rule out these other possibilities, you may undergo multiple tests, including laboratory tests (such as cobalt and chromium levels), X-rays, a bone scan, and a biopsy.
The American Contact Dermatology Society has defined criteria for diagnosis of Post Implantation Metal Hypersensitivity Contact Dermatitis in patients with unexplained pain and/or failure of the offending implant:
Major criteria
- Eruption overlying the metal implant
- Positive patch test reaction to a metal used in the implant
- Complete recovery after removal of the offending implant
- Chronic dermatitis beginning weeks to months after metallic implantation
Minor criteria
- Dermatitis reaction is resistant to therapy
- Morphology consistent with dermatitis (erythema, induration, papules, vesicles)
- Systemic allergic dermatitis reaction
- Histology consistent with allergic contact dermatitis
- Positive in vitro test to metals (e.g., lymphocytes transformation test)
What is an allergic patch test for allergic contact dermatitis?
Patch testing is commonly used to detect allergic contact dermatitis to metals. It is a test performed by testing your skin with small doses of the irritant. The sensitivity and specificity of this test are only 77% and 71% for determining if a patient has a hypersensitivity to metal. An allergic reaction at the skin level may not necessarily correspond to an allergic reaction at the bone or muscle layer level.
If you are interested in patch testing, schedule an appointment at our office for Sensiband testing.
The Sensiband is an innovative wristband designed to test for metal allergies, a critical consideration for individuals preparing for joint replacement surgeries. It holds interchangeable discs made of medically pure metals, including Nickel, Cobalt, Chromium, Titanium, Molybdenum, Aluminum, and Copper, against the skin for up to a week. This first-of-its-kind, patented wearable metal test kit enables users to identify potential allergic reactions to the metals commonly used in joint replacements, dental implants, and other medical procedures. The process is straightforward: if a user develops a skin reaction like contact dermatitis while wearing the band, it suggests an allergy to the particular metal in contact with their skin. This vital information can be communicated to surgeons before procedures involving metal implants, such as knee or hip replacements. The Sensiband thus offers a simple, cost-effective, and efficient method for preoperative allergy testing, helping to prevent serious postoperative complications associated with metal hypersensitivity.

What is the lab test for a metal allergy following knee replacement?
The most accurate test available is the lymphocyte transformation test. This blood test compares the number of white blood cells created after seven days with and without exposure to metal. It is more sensitive than the patch test alone.
Orthopedic Analysis offers two primary testing panels for metal hypersensitivity, crucial for identifying and managing metal allergies in patients, especially those undergoing orthopedic surgeries. Here are the details of these testing panels:
Key Points on Orthopedic Analysis Testing Panels
Panel 1: Standard Metal Panel
Metals Tested: This panel typically includes tests for common metals used in orthopedic implants, such as nickel, chromium, cobalt, titanium, and sometimes additional metals like molybdenum, vanadium, and zirconium.
Purpose: It is designed to identify hypersensitivity reactions to the most commonly used metals in orthopedic devices, helping clinicians select appropriate implant materials for patients.
Panel 2: Comprehensive Metal Panel
Metals Tested: This panel is more extensive and includes a broader range of metals, such as bone cement monomers, and those tested in Panel 1. It may also include tests for other alloy components like iron and specific alloy particles (e.g., cobalt alloy, titanium alloy).
Purpose: This panel is used for patients who require a more detailed assessment, especially those with complex histories of implant failures or multiple sensitivities. It helps identify specific allergens that could be causing adverse reactions, including reactions to bone cement components.
Additional Information
Testing Methodology: Both panels use the Metal-Lymphocyte Transformation Test (Metal-LTT), a blood test that measures the immune cell response to different metals. This test is highly quantitative and provides detailed results on the level of reactivity to each metal tested.
Clinical Use: Clinicians use the results from these panels to make informed decisions about implant selection, revision surgeries, and patient management strategies to avoid adverse reactions to metal implants.
Is the lab test for metal allergies covered by insurance?
Medicare generally does not cover the Lymphocyte Transformation Test (LTT) for metal hypersensitivity testing, such as those offered by Orthopedic Analysis, for the following reasons:
- Specific Coverage Limitations: Medicare only covers the Lymphocyte Transformation Test (CPT code 86353) for particular purposes, such as organ transplant or monitoring of immunotherapy, and not for metal hypersensitivity testing.
- Insurance Coverage: Most third-party payers do not cover this testing due to its non-FDA-approved status.
- Lack of FDA Approval: The LTT-MELISA test, commonly used for detecting metal sensitivity, is not FDA-approved for this specific indication. This lack of approval is a significant factor in insurance companies not covering the test. If the LTT is classified as a Laboratory Developed Test (LDT), it does not require FDA approval, clearance, or emergency use authorization. However, it must comply with the Clinical Laboratory Improvement Amendments (CLIA) of 1988 and its implementing regulations. Laboratories can develop, validate, and perform these tests without FDA oversight, but they must ensure the test meets CLIA standards. Orthopedic Analysis provides its CLIA certificate on its website.
- Logistical and Validation Issues: The test also faces logistical challenges, such as the need for viable lymphocytes and limited availability, which further complicates its acceptance and coverage by insurance providers
Scheduling a Metal Allergy Test
Book an appointment with Dr. Morton to order these tests. You may also request the test kit directly from Orthopedic Analysis and have us perform the blood draw. You will have to cover the cost of overnight shipping from Hawaii.

What does the x-ray for a hypersensitivity response for a knee replacement look like?
X-rays in patients with metal hypersensitivity reactions often look normal. Sometimes there is osteolysis (loss of bone) around the metal implants on x-ray. This loss of bone can sometimes lead to severe loosening of the components and failure of the knee replacement.

What do biopsies of metal allergies look like?
Often, during implant removal, intra-operative biopsies are obtained. These biopsies usually demonstrate increased lymphocyte infiltration into the synovial tissue. The synovial tissue is the tissue found within the knee joint responsible for generating fluid in the knee (synovial fluid). Often, the synovial tissue will show granulation tissue, fibrosis, numerous giant cells, and calcification. These findings are consistent with a chronic inflammatory response.
What are the treatments for nickel allergy after knee replacement?
Many patients demonstrate improvements following short-term therapy with topical steroid medication for the rash. Anti-inflammatory medications and physical therapy may treat the symptoms of synovitis (inflamed tissue).
If symptoms do not resolve, revision surgery with a hypoallergenic implant may be considered.
Symptoms should resolve two to three months after revision surgery.
What are the possible alternatives to nickel implants in total knee replacement surgery?
Several manufacturers provide alternative knees for hypersensitive patients. Options include adding a coated layer on cobalt-chromium, ceramic-covered, and titanium implants. Most of these implants are designed to minimize allergic reactions to nickel.
Coated implants add a coating layer over the implant to prevent exposure to the underlying metals. Standard coating options include Titanium-nitride (TiN), Zirconia Nitride, and Titanium Nobium. Studies of these implants demonstrate that some have a higher revision rate (sometimes 91% at 5 years). At revision, implant-retrieval studies demonstrate that 20% of these implants have coating delamination and exposure to the deeper layers. This may cause nickel release and lead to a continued immune response.
Ceramic implants include oxidized zirconia (Oxinium). This implant utilizes a femur that is coated with oxinium and a tibia that is made of titanium, thus avoiding nickel allergy issues. Concerns arise from the Australian Joint Registry, where 12-year outcomes demonstrate a 2x higher risk for revision in Oxinium knees. This is similar to the American Joint Registry evaluating 7-year data of these implants. A recent study in 2023 demonstrated that there may actually be an increase in nickel during implantation of these components.
Titanium implants may undergo a hardening process that creates a nitrogen-enriched zone on the surface of a titanium femur component. Interestingly, implants that undergo this process demonstrate a 96% reduction in wear rates compared to conventional implants and may lead to longer-lasting implants. This is the implant of choice for Dr. Morton in patients who are concerned of a metal allergy. Read more about Ti-Nidium here.
Do I need a hypoallergenic knee replacement if I do not have a history of metal allergies?
In patients who do not have an allergy before surgery do not necessarily require a hypoallergenic knee replacement. The available tests are unreliable. Furthermore, there may be some concern regarding these implants’ longevity and clinical performance. If you do have an allergic contact dermatitis reaction to nickel, you discuss this with Dr. Morton, and you may be a candidate for a hypoallergenic knee replacement.
Should I consider a revision knee replacement if I have a painful knee replacement?
Success rates for revision knee replacement where there is a strong suggestion of a metal allergy are variable. Several case series have demonstrated successful treatment of metal allergy with revision to a knee replacement without nickel. There are also reports of patients who do not do well with the surgery. Discuss with Dr. Morton if you would be a candidate for revision knee replacement.
Conclusion
If you are considering a total knee replacement and have a metal allergy or sensitivity, speak with Dr. Morton about possible alternatives. Several manufacturers provide alternative knees for patients who are allergic to nickel, but they come with their own set of drawbacks. If you had a knee replacement and believe that you may have a hypersensitivity reaction, schedule an appointment with Dr. Morton today.
References:
Granchi D, Cenni E, Giunti A, Baldini N. Metal hypersensitivity testing in patients undergoing joint replacement: a systematic review. The Journal of bone and joint surgery. British volume. 2012 Aug;94(8):1126-34.
Lawrie CM, Bartosiak KA, Barrack TN, Nunley RM, Wright RW, Barrack RL. James A. Rand Young Investigator’s Award: Questioning the “Nickel Free” Total Knee Arthroplasty. J Arthroplasty. 2022 Aug;37(8S):S705-S709. doi: 10.1016/j.arth.2022.03.058. Epub 2022 Apr 2. PMID: 35378232.
Matar HE, Porter PJ, Porter ML. Metal allergy in primary and revision total knee arthroplasty : a scoping review and evidence-based practical approach. Bone Jt Open. 2021 Oct;2(10):785-795. doi: 10.1302/2633-1462.210.BJO-2021-0098.R1. PMID: 34587776; PMCID: PMC8558451.
Saccomanno MF, Sircana G, Masci G, Cazzato G, Florio M, Capasso L, Passiatore M, Autore G, Maccauro G, Pola E. Allergy in total knee replacement surgery: Is it a real problem? World J Orthop. 2019 Feb 18;10(2):63-70. doi: 10.5312/wjo.v10.i2.63. PMID: 30788223; PMCID: PMC6379738.
Samuel Akil, Jared M. Newman, Neil V. Shah, Natasha Ahmed, Ajit J. Deshmukh, Aditya V. Maheshwari, Metal hypersensitivity in total hip and knee arthroplasty: Current concepts, Journal of Clinical Orthopaedics and Trauma, Volume 9, Issue 1, 2018, Pages 3-6, ISSN 0976-5662, https://doi.org/10.1016/j.jcot.2017.10.003.