Get Your Hip or Knee Injection Today!
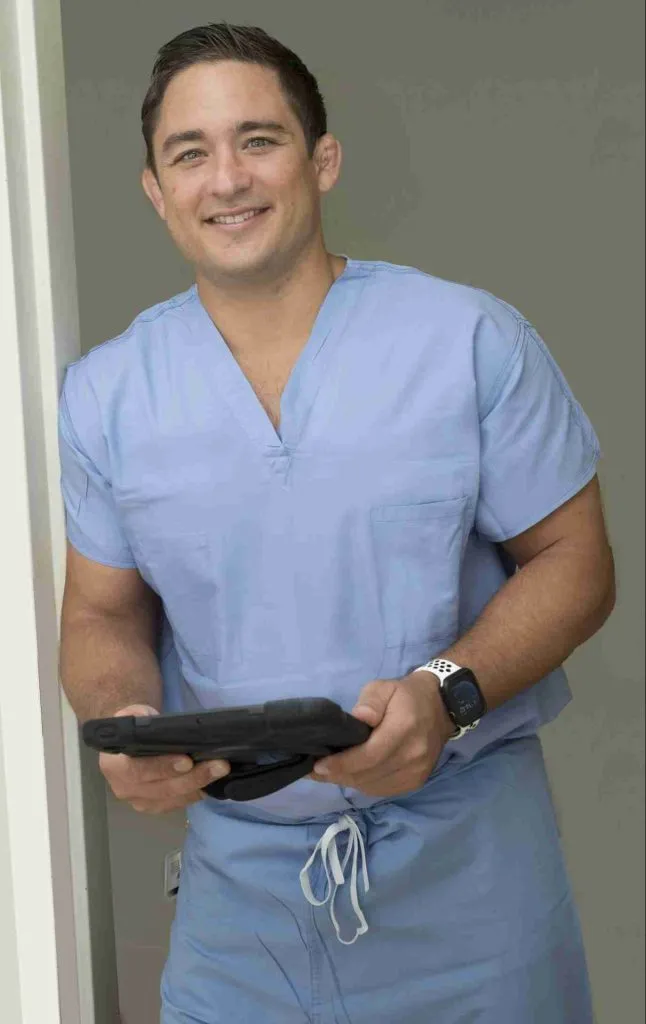
Choose Dr. Morton as Your Hip or Knee Injection Doctor
- Experienced Orthopedic Surgeon
- Nonoperative and operative treatments available
- High success rate in providing joint injections
- Excellent nonoperative treatments for arthritis available
- Well-versed with modern techniques
- Evidence-based injections, not driven by industry and marketing
- Fellowship-trained in joint replacements
- Platelet Rich Plasma (PRP)
- Steroid Injections
- Hyaluronic Acid (gel) Injections
- Ultrasound guided
- Alternatives to Knee and Hip Replacement
Joint injections are common orthopedic procedures. Your surgeon may provide you with a joint injection for various reasons including diagnosis, pain, and therapeutic treatment. There are various types of injections offered in different locations. Injections are often lower risk compared to surgical intervention. It is an excellent intervention for hip and knee arthritis.

Types of Injections
Corticosteroid Injections
Steroid injections are typically composed of an anesthetic such as lidocaine and/or marcaine as well as the selected steroid. The lidocaine and marcaine take effect almost immediately and can provide relief for several hours. Typically if pain is relieved during this time, then we are addressing the appropriate pain generator. The steroid portion of the injection often takes 2-3 days to begin to take effect and lasts 3 months on average. There are no formal limits on the number of steroid injections one can receive into a joint. Most orthopedic surgeons suggest not receiving more than 4 injections per year.
Adverse Reactions: Overall injections are considered to be safe – with very few problems.
- Infection – This is an extremely rare, but sometimes severe complications. If you have redness and severe pain following an injection – please seek emergency care.
- Steroid flare – Sometimes patients experience an elevation in pain the day after a steroid injection. This often resolves over the course of 24 hours.
- Elevation in blood glucose – Patients who undergo a steroid injection with a history of diabetes are encouraged to monitor their blood sugar levels and expect an increase over the next three days.
How Steroid Injections work:
Cortisol is a hormone naturally produced by the body during stress (fight or flight response). This is done to suppress the inflammatory response during stress. Cortisone is a strong anti-inflammatory that works in a similar fashion, suppressing the inflammatory system, and thus naturally produced pain generators.
Concern regarding degenerative effects on cartilage:
There are conflicting data regarding whether cortisone injections cause worsening arthritis. There are some studies demonstrating worse arthritis in 6% of patients after a steroid injection. The studies on damage due to steroid injections is not well done and is unreliable. These studies are unable to prove that the arthritis is worsening because of the injections, or if the study recipients already had worsening arthritis in spite of these steroid injections. This is why most physicians provide a balanced view on providing steroid injections on a limited bases of no more than 3 – 4 per year per joint.
Hyaluronic acid or gel injections are provided by many manufacturers. The original hyaluronic acid injections were derived from rooster comb. Gel injections theoretically act like a lubricant and shock absorber. The gel decreases swelling and friction, ultimately reducing pain There are now synthetic alternatives that exist to avoid allergic reactions to animal products. There is conflicting evidence regarding the efficacy of these types of injections. It is approved for knee arthritis injections.
Adverse Reactions:
- Infection – This is an extremely rare, but sometimes severe complications. If you have redness and severe pain following an injection – please seek emergency care.
- Gel Reaction – The increase in the amount of fluid in the knee can cause severe pain.
Toradol
An alternative to steroid injections1. This medication works along a similar pathway to reduce pain. This is a less common injection modality. Research has investigated its use in knee osteoarthritis and subacromial bursitis. It is a good alternative to steroid injections as it will not provide an elevation in blood glucose and is a good option in patients with diabetes.
Adverse Reactions:
- Infection – This is an extremely rare, but sometimes severe complications. If you have redness and severe pain following an injection – please seek emergency care.
- Allergic reaction may occur.
- Tests have not been performed in patients who have had poor tolerance to oral NSAIDs or have renal abnormalities.
- SM MCGowan, WE Rodriguez, T Visser, V Yellapu, PN Morton, GF Carolan, “A randomized Double-blind Study Comparing Intra-articular Corticosteroid to Intra-articular Ketorolac Knee Injections.” St Luke’s University and Health Network. AAOS, Mar 2019
Platelet Rich Plasma or PRP is a newer injection that has recently become more available. Several studies have shown that it is helpful in the treatment of arthritis. Often, patients have improvements in their pain for 6 months or greater. PRP may also be an alternative for patients who are experiencing certain types of tendinopathy. PRP is may cost more and insurance may not cover this procedure. Dr. Morton’s office provides PRP injections. Call today to schedule.
Stem Cell Injections
There are many advertisements for stem cell injections for orthopedic problems. This is considered very experimental for osteoarthritis. Many studies on stem cell injections have been done, showing minimal improvement. No studies have demonstrated significantly successful treatment of orthopedic issues with stem cells. These are often expensive.
Injection Sites
Knee
There are many locations around the knee that can be injected, including the knee joint, Illiotibial band, and pes-anserine bursa. Types of injections include corticosteroids, hyaluronic acid, and Toradol. The knee joint is commonly injected four times per year every three months without issue for as long as a patient desires with minimal risk.
Hip
Often the hip can be injected either into the hip joint, greater trochanteric bursa, or iliopsoas tendon. Hip joint or iliopsoas injections require visualization with either fluoroscopy or ultrasound in order to determine accuracy. Typical injections include corticosteroid injections. Similar to a knee injection, the joint may injected every three months without issue for as long as a patient desires with minimal risk.
Shoulder
The shoulder is a complex joint that is comprised of different components. You may receive an injection to the subacromial bursa, glenohumeral joint, and biceps tendon. Typical injection components may be either steroid or Toradol injections.
Nerve Compression or Tendinopathies
Occasionally a one-time steroid injection may be provided to tendinopathies such as de Quervain’s tenosynovitis or trigger finger. Multiple injections in these areas lead to concerns of tendon rupture. Similarly, a steroid injection can be provided to nerve compression problems such as carpal tunnel. Some tendinopathies may be amenable to PRP injections. Surgical treatment is often recommended when steroid injections fail.
Small-to-Medium Sized Joints
Injection Delivery
There are different methods of getting an injection. Essentially, higher levels of technology are utilized to get better accuracy. Most commonly, patients receive an injection in the clinic. These injections are called “landmark injections”. Sometimes in the clinic, you may receive an injection with ultrasound guidance. These are called “ultrasound-guided injections”. X-ray technology can be used to help guide an injection. These injections are known as “fluoroscopic-guided” injection. Some injections require a 3-dimensional CT scan to make sure that injections are in the right place.

Landmark-Based Injections
Landmark-based injections are injections that require the lowest level of accuracy. This is because the landmarks used are thought to provide a reliable way to access the joint. Using the knee joint as an example, the kneecap, thigh-bone (femur), and shin-bone (tibia) are used to determine where to place the injection. Steroid injections are reliable in this setting because the knee joint a large encapsulated area and steroid medications will be able to diffuse throughout the knee.
Ultra-Sound Guided Injections
Sometimes image-guided injections are required in order to provide a more accurate injection. Even in the knee joint, sometimes a more accurate injection is required. Hyaluronic acid injections (gel shots), PRP, and stem-cell injections require 100% accuracy to ensure that the injections are within the capsule. Unlike steroid injections, these medications are unable to diffuse through the capsule of the joint.
X-Ray Injection (Fluoroscopic–Guided)
Soft-tissue often gets in the way of seeing the joint. The hip joint is a common area to use an x-ray to inject. In patients who are larger, it can be difficult to see the needle enter into the joint without an x-ray.
Aspiration
Sometimes, for a very swollen knee, your doctor will perform an aspiration. Aspiration involves removing fluid from your knee. This process is fairly simple where your doctor will first numb up your knee and then remove your fluid from the knee. Sometimes, the fluid is sent for testing. After the fluid removal, your doctor will then put the medication into your knee joint.
Pain relief from an aspiration occurs due to the joint becoming decompressed.

Tests
If your doctor is concerned regarding gout, they may send your fluid for crystals. The crystals are looked at under a microscope, and their presence would confirm the diagnosis.
Similarly, if your doctor is concerned for infection, the tests will analyze for white blood cells. It is unlikely that your doctor would perform an injection if they are concerned for infection at this point.
If you have any questions regarding your injection, do not hesitate to call Dr. Morton at (808)548-7033. He has the ability to perform in-office ultra-sound injections to ensure the accuracy of your injections.
To read more about hip or knee arthritis, click here.
Frequently Asked Questions Of Joint Injections(FAQ)
There has been no study to substantiate that injections of PRP or stem cells will rebuild the cartilage in your knee. If you find a study, I am happy to review the science with you.
You can resume normal activities. I usually advise people to avoid strenuous activity such as jogging or lifting on the day of injection. You can resume all higher levels of activity the following day.
There is a small amount of discomfort associated with orthopedic injections. I do my best to minimize this discomfort by using either a “cold spray” or a lidocaine injection. Most patients say that it was a lot less painful than anticipated.
The best-studied medication for injections is steroid injections. Orthopedic surgeons have a long history of successful steroid injection use. The studies supporting other types of injections are not as strong and should be approached with more caution.
For joints and bursa injections such as those located on knees or hips, I am happy to perform the injection every 3 months. For tendon or nerve injections, I rarely inject more than once. This is because we know that it is safe to inject steroids into joints. There is a concern with tendon rupture with multiple steroid injections.
Related Pages
Personalized Alignment In Knee Replacement Surgery
Knee replacement surgery has long been a solution for patients who have severe arthritis or joint degeneration. Traditionally, the procedure has involved using standardized techniques to position the knee implant. However, personalized alignment in knee [...]
Hiking After Knee Replacement: Tips for Staying Active
Knee replacement surgery can be life-changing, offering significant relief from pain and improved mobility. However, returning to physical activities like hiking may seem daunting for many. However, hiking after knee replacement is possible—and even beneficial [...]
Uncemented Knee Replacement: What Patients Should Know
Knee replacement surgery has evolved significantly over the years, with various techniques and approaches tailored to meet individual patient needs. Among these, uncemented knee replacement is gaining attention as an alternative to the traditional [...]
How Much Does A Hip Or Knee Replacement Cost?
Understanding Your Expected Bills Hip or knee replacement surgery is a transformative procedure that can significantly improve the quality of life for individuals with severe arthritis or joint damage. However, the financial aspect [...]
Cost of Total Knee Replacement in Hawaii for Medicare Patients: How to Save Money with Outpatient Surgery Centers
Total knee replacement (TKA) is a life-changing procedure for patients suffering from severe arthritis or knee dysfunction. With advancements in surgical techniques, many TKAs are now performed on an outpatient basis, allowing patients to [...]
Understanding Post-Traumatic Arthritis After ACL Reconstruction
Anterior Cruciate Ligament (ACL) injuries are a common occurrence, especially among athletes and physically active individuals. While ACL reconstruction is a widely accepted procedure to restore knee stability and function, it is important to [...]