Table of Contents
Total hip arthroplasties are one of the most common and most successful surgeries of our time. A new hip joint can decrease your pain and give you your life back. But of course, there is still the risk of a painful hip replacement.
Nearly 96% of people who undergo hip replacement surgery report complete satisfaction, even 16 years after surgery! A smaller number of people, ranging from 12% up to 18% (depending on what study you look at), have continued pain. In most cases, it is linked to the femoral component (the stem that is placed in your upper thigh bone). But there are several reasons why one may still experience pain after a total hip arthroplasty. Let’s take a look at some of the most common causes.
Causes of A Painful Total Hip Arthroplasty
Intrinsic Causes- coming from inside of the hip joint:
- Loosening
- Infection
- Instability
- Impingement
- Metal Sensitivity
Extrinsic Causes- coming from outside of the hip joint:
- Trochanteric Pain Syndrome
- Insufficiency Fractures
- Spinal Pathology
- Post-Surgical Pain Syndrome
- Other causes known to refer pain to the hip
Intrinsic Causes
Loosening
In some cases, the cup and or stem of the replacement may become loose, requiring revision surgery of the hip replacement. Loosening of the implants can occur shortly after surgery or even years later.
If the acetabular portion of the replacement, known as the cup, becomes loose, you may experience groin and buttock pain. If the femoral part of the replacement, known as the stem, becomes loose, you may note thigh pain and sometimes pain in the groin.
So many factors come into play when it comes to what may cause an implant to loosen. The incorrect size of fitting, how much activity or weight-bearing activity a person participates in, the age of the person receiving the new hip, and possibly the type of implant, either cemented or uncemented. As of now, research has not determined if cement or uncemented hip replacements are more likely to become loose. But, as research evolves and advances, we may learn more about this.
Imaging and a detailed history of activity level and pain presentation can help your surgeon determine the best treatment option, including revising the hip replacement.

Prosthetic Joint Infection

Unfortunately, any surgery runs the risk of infection. For total hip replacements, this ranges from a superficial infection of the incision (cellulitis) or a deep infection around the implant, known as prosthetic joint infection. However, the incidence of this deep infection is relatively low, less than 1%.
Just as the new hip joint can loosen due to improper sizing, or lack of ingrowth, a prosthetic joint infection can also cause the implant’s loosening.
Laboratory tests, biopsy, and imaging can help confirm infection, allowing your medical team to treat you properly.
One may be more prone to infection of the newly replaced hip if they have any of the following risk factors:
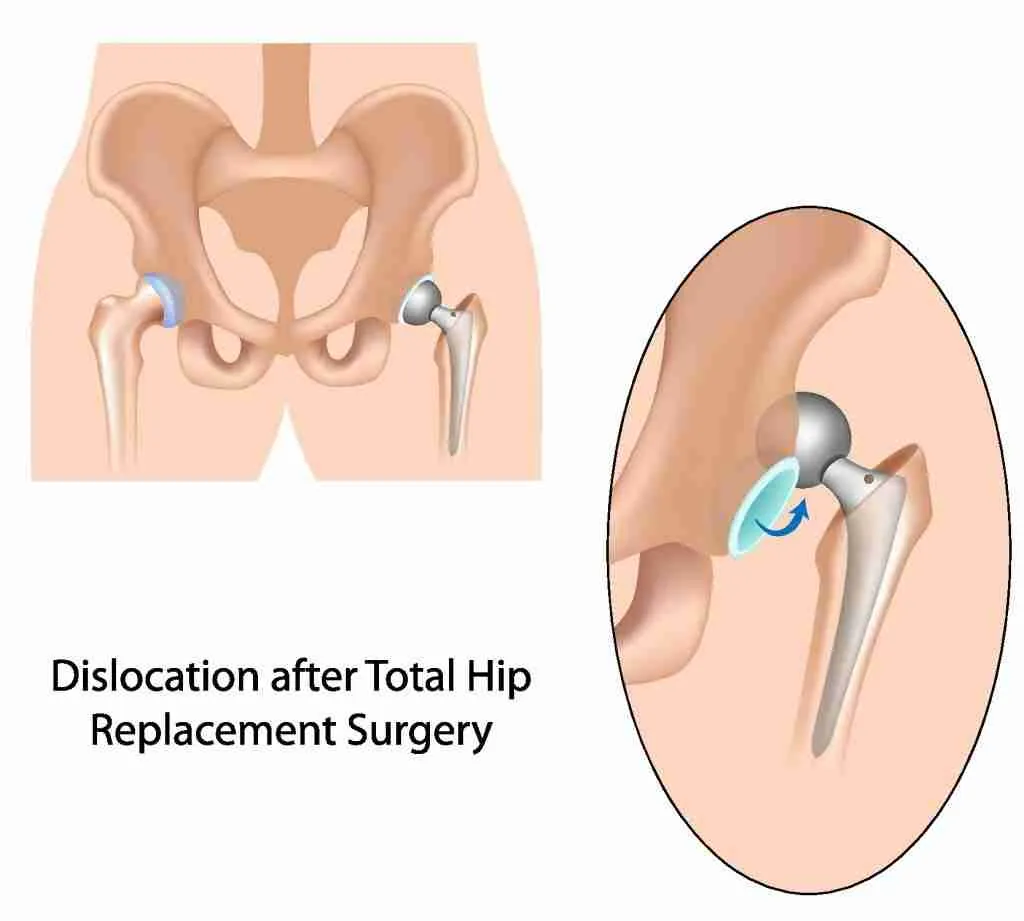
Instability
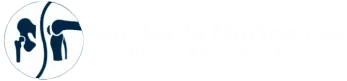
Instability of the hip joint may also be caused by improper fitting or placement of the prosthetic implants. However, not following through with post-operative guidelines (in posterior hip replacements) can put you at risk for instability or dislocation. Improving the strength and function of the core and hip can help improve hip stability. Instability can be caused by poor position of the implants, spine issues, and other medical conditions that put you at risk. Revision surgery is sometimes required to correct the instability.
Impingement
Impingement of your hip replacement can occur due to improper implant sizing or soft tissue irritation. Implants that are sized too large can cause your tendons to become overstretched and irritated. Conversely, implants that are sized too small can cause your tendons to be under-tensioned and lead to dislocation. Impingement can cause pain of the groin, front of your hip, and even into your thigh or buttock.
Physical therapy can help with strengthening and stretching your musculature. Occasionally, you may require revision to ensure the implants fit correctly and establish a pain-free range of motion. Sometimes conservative treatment such as Physical Therapy can help improve your symptoms, allowing you to experience decreased pain and improved function.
Metal Sensitivity

Unexplained pain after a hip replacement can sometimes be from a reaction to the replacement components. Metal-on-metal components are a discontinued hip replacement that many surgeons thought would last longer. Unfortunately, these hip replacements have had early failures and need to be revised.
Lab results can help detect your metal ion levels if this is the case. Imaging, including both x-rays and MRIs, can see this sensitivity and associated inflammation by assessing the synovial or joint lining thickness and volume. Revision surgery is required to remove the components to replace them with something better tolerated by the patient.
Extrinsic Causes
Extrinsic causes of a painful total hip arthroplasty happen outside of the hip joint and are not directly related to the implant itself. As you may have realized already, all of the intrinsic reasons revolve around the implants.
Extrinsic causes of pain after a total hip arthroplasty can often be treated with more conservative measures.
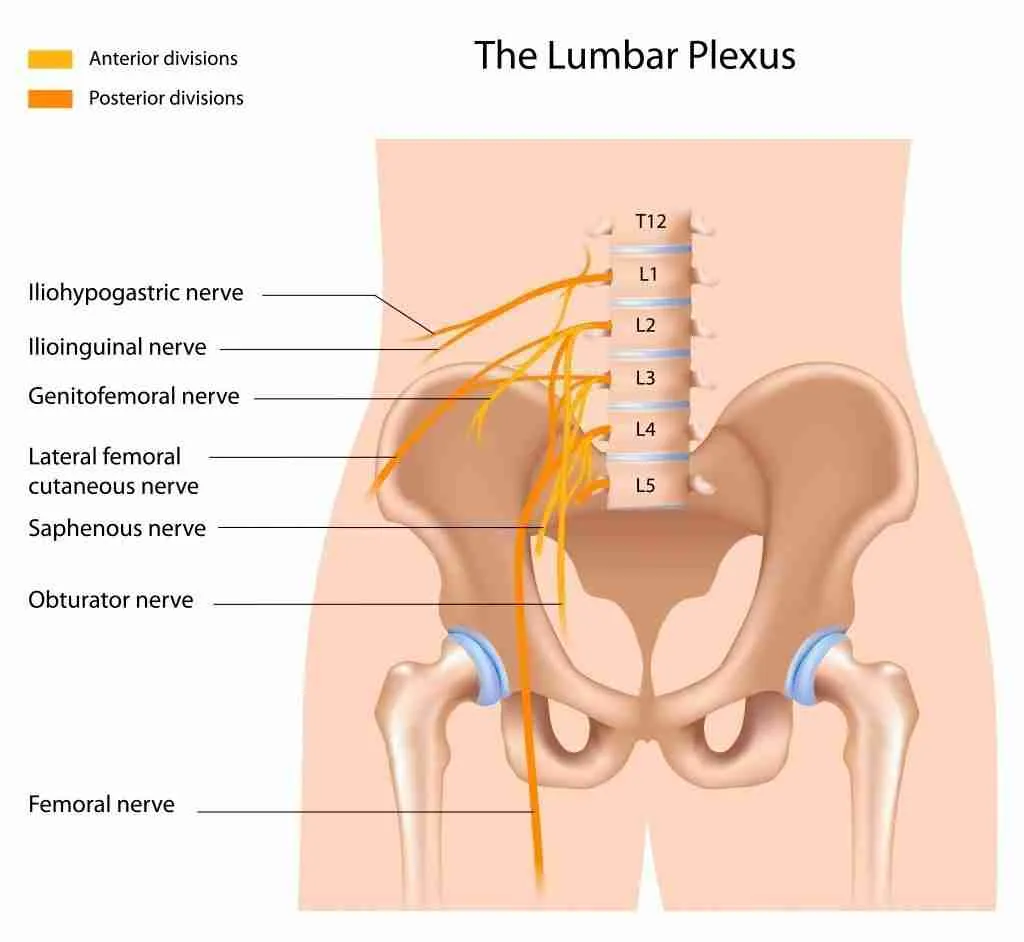
Lateral Femoral Cutaneous Nerve
During the anterior approach to a hip replacement, the lateral femoral cutaneous nerve travels near the incision. The nerve can be stretched or cut during surgery. Injury to the nerve can cause numbness to the thigh region. Sometimes the damage can create a neuroma, which can become painful.
Some surgeons routinely cut the nerve during an extensive surgical approach to the hip. Dr. Morton is a fellowship-trained hip specialist and is careful to minimize this risk as much as possible by performing a minimally invasive procedure.
Suppose you are having pain or numbness to your anterior thigh. In that case, a physical examination will help determine if this is the cause.
Trochanteric Pain Syndrome
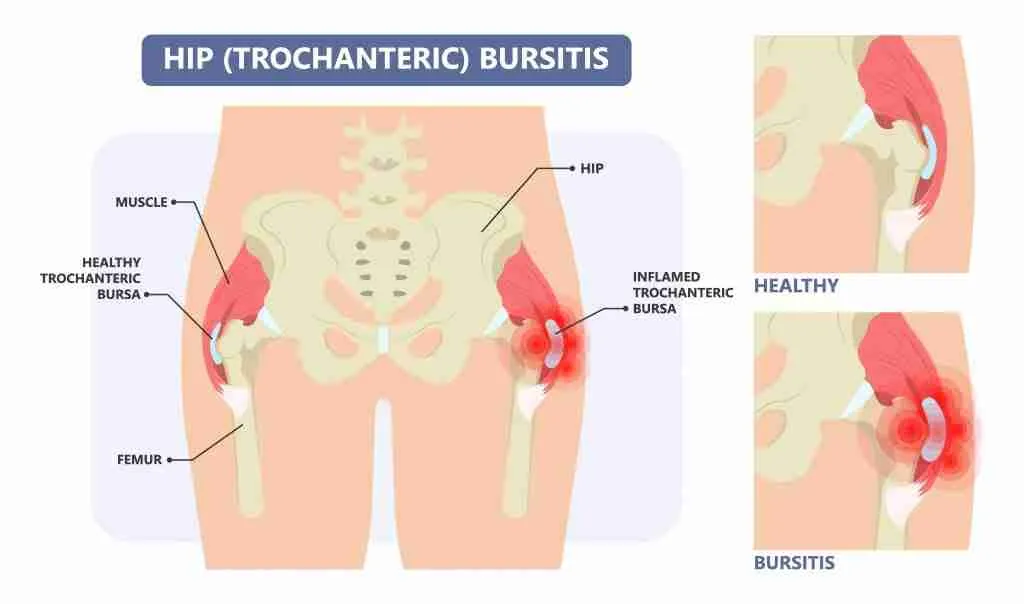
Your trochanter is a bony prominence of your hip bone, the most prominent portion of bone that you can feel on the outside of your hip. Many tendons and bursa reside near this trochanter.
The tightness of your buttock muscles can cause constant pressure to the outside of the hip, leading to pain and inflammation. When you walk, sit, and lay down on your hip, this can cause continued stress and irritation.
The trauma and inflammation associated with total hip replacement surgery can also irritate the trochanteric region, creating pain with nearly every regular, daily activity. Physical therapy involving stretching and strengthening of the musculature around this area can improve the pain. Dr. Morton can give you a steroid injection to help with your soreness and inflammation.
If there is a weakness to your hip that does not improve with therapy, your hip can be evaluated for a gluteus medius tear. The gluteus medius is a buttock muscle that is important to normal walking and can be painful if partially torn or cause a limp if it is completely torn.
A thorough exam and imaging can help diagnose you and develop a plan of care to help decrease stress to the outside of your hip while improving flexibility and strength.
Insufficiency fractures
Insufficiency fractures are small fractures or stress fractures without a known mechanism or known trauma to an area. These fractures come on due to a change in weight-bearing status and activity level that is too much for the new implant’s bone.
Without warning, patients can begin to note pain in their hip, thigh, or even pelvis. Unfortunately, these fractures can occur at sites away from the replacement site, such as into the pubic ramus or other parts of the pelvis due to the changes in stress and load that comes with the newly replaced hip.
Upon imaging, these fractures can be detected and treated appropriately. Rest or operative fixation surgery may be necessary if the fractures do not heal on their own.

Spinal Pathology
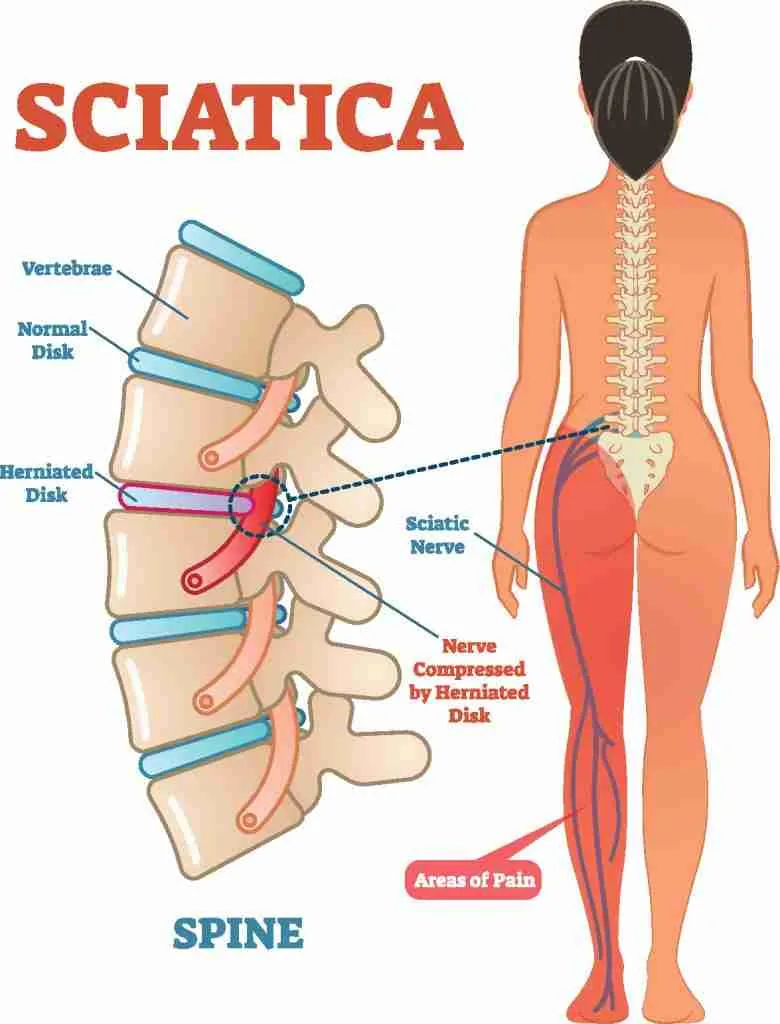
Degeneration of the spine can also mimic pain at the hip. Nerves that travel down to the hip may be impinged or inflamed, resulting in pain and dysfunction. Even the sacroiliac joint (SI joint) can refer pain to the hip if it is not moving or functioning optimally.
At times chronic hip pain and osteoarthritis can lead to spine dysfunction due to the years and years of abnormal gait and movement patterns. Thus, it is essential to treat the whole person both before and after surgery to determine if the pain is secondary to spine problems.
Persistent Post-Surgical Pain
There are times when some people continue to have persistent post-surgical pain after undergoing a total hip arthroplasty. Between 6 and 27% of people experience this. When no known causes are identified, and there is no explanation for your continued pain, you may be referred to a pain management specialist. Pain management doctors can be helpful with treating pain that may not be secondary to your hip replacement.
Deciding to have a total hip arthroplasty is exciting and is usually a very positive experience. If you are having issues with your hip replacement, schedule a consultation with Dr. Morton.